Expert Opinion on Published Articles
Abstract
The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. A new method
Rainer Baumgart
Oper Ortho Traumatol 2009;21:221-233.
DOI 10.1007/s00064-009-1709-4
Limb length discrepancies have an effect on gait economy and may have long-term consequences for surrounding joints. Surgical procedures for correcting these length discrepancies are becoming more established and are increasingly being performed by general orthopaedic surgeons. It is however important to understand the effect that lengthening will have on the mechanical axis of the limb and to correct or maintain joint orientations to avoid secondary deformities.
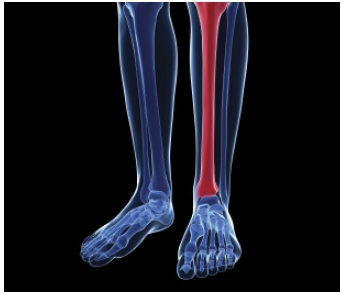
Limb-lengthening procedures are predominantly performed with external fixators that can lengthen along the mechanical axis of a bone segment and thereby maintain the orientation of the adjacent joints and overall alignment of the limb. Due to the morbidity associated with the long-term use of external fixators, lengthening with motorised intramedullary devices is gaining popularity. These devices are implanted in the medullary canal, which approximates the anatomical axis of the bone segment, and lengthening along this axis may cause secondary deformities. This is particularly relevant when lengthening the femur, where lengthening along the anatomical axis will result in axis deviation and distal femoral valgus, and affect the overall alignment of the entire limb.
Where limb length discrepancies are associated with angular deformities, the implications of lengthening on overall limb alignment become even more complex. External fixators allow the gradual correction of deformities and lengthening along the mechanical axis until a desired endpoint has been achieved. The use of motorised intramedullary devices on the other hand requires the acute correction of angular deformities prior to lengthening while simultaneously keeping the effect of lengthening on final joint alignment in mind.
Dr Baumgart's article presents a new method for the planning of limb-lengthening procedures of the lower limb with or without deformity correction and is a must-read for any surgeon contemplating intramedullary lengthening of the lower limb. The author illustrates a step-by-step approach of the proposed method for four clinical scenarios including: antegrade nailing of a femur; retrograde nailing of a femur; antegrade nailing of a tibia; and a combined approach for concomitant femoral and tibial deformities. The article explains the pre-operative planning in detail and also provides a clear description of the surgical technique. The proposed technique is described with the use of the Fitbone® intramedullary lengthening nail (Fitbone®, Wittenstein Company, Igersheim, Germany) but can be used with any motorised lengthening nail or 'lengthening over a nail' procedure.
The original article was published in 2009 but the idea failed to find fertile ground among orthopaedic limb reconstruction surgeons until now. This was partly due to a radical paradigm shift - from gradual deformity correction and lengthening with an external fixator to acute correction and lengthening with a nail - that was required in the field of limb reconstruction surgery and the lack of commercially available motorised lengthening nails.
With motorised lengthening nails, like the Precice® nail (Ellipse Technologies, Inc, Irvine, CA, USA), becoming more readily available, surgeons are looking towards this technology for managing leg length discrepancy. This has led to a renewed interest in the effects of lengthening along the anatomical axis and the Reverse Planning Method of Dr Baumgart.
Reviewer: Prof JA Shipley
Professor Emeritus
University of the Free State
Bloemfontein
Comparison of clinical outcomes and cost effectiveness of percutaneous wire and locking volar plate fixation of Colles' fractures
Comparative studies of traditional Kirschner wire and modern locking volar plate fixation of distal radius fractures are uncommon. The proposed benefits of volar plates include better radiological outcomes, more rigid fixation with earlier return of function, fewer wound complications and reduced need for additional services such as POP changes, physiotherapy and outpatient visits. By ensuring anatomical restoration, future disability should theoretically be reduced. As a result there has been a massive swing towards the use of volar locking plates for these fractures despite the additional costs involved and the potential for new problems such as tendon damage, deep infection and need for plate removal.
Two recent well-conducted trials in the UK have uniquely compared not only the clinical outcomes of the two techniques, but also their cost effectiveness. The clinical and financial analyses were published separately for each trial, but I think it is important to combine them to gain an overall picture of the balance between cost and possible clinical benefit.
In summary it appears that the use of locking volar plates costs approximately R15 500 (GB £713) more per case for little or no clinical benefit in the average Colles' fracture requiring fixation to maintain reduction. The only significant benefit appears to be earlier recovery of function at 6 weeks, and the conclusion from both series is that volar plates are not cost effective in the context of the UK National Health Service. I have no doubt that there are situations where a volar plate is the better option, but they need to be adequately defined to justify the additional expense.
1. Surgical treatment of distal radius fractures with a volar locking plate versus conventional percutaneous methods: a randomised controlled trial
Karantara et al. J Bone Joint Surg (Am) 2013;95-A:1737-44
2. Cost effectiveness of volar locking plate versus percutaneous fixation for distal radial fractures
Karantara et al. Bone Joint J 2015;97-B:9:1264-70
These two articles are analyses of clinical outcomes and cost effectiveness of the same group of 130 patients treated in a prospective randomised controlled trial for dorsally displaced distal radius fractures at a single centre. Percutaneous fixation with Kirschner wires was used in 64 patients; 11 of them had additional bridging external fixation. Volar locking plates were used in 66 patients. Patients were assessed at recruitment, 6 weeks, 12 weeks and 1 year after surgery using the Patient Evaluation Measure (PEM), QuickDASH and EQ5D questionnaires. Data on operating times, outpatient visits, additional procedures or physiotherapy, cost of treating complications and days off work were collected. The study was designed to take account of the hidden costs of percutaneous fixation and not simply the difference in the price of implants.
Surprisingly there was no difference in operating times; the authors suggest this may be due to radiography delays; it is probable that additional cost benefits of percutaneous fixation would be gained by improving theatre efficiency. There were fewer complications in the plate group; only two developed infections, but two patients did require plate removal. In comparison, the percutaneous group had five infections, one delayed carpal tunnel decompression, one EPL reconstruction (after revision to a plate for failure of percutaneous fixation) and two patients needed removal of buried wires, but these differences were not statistically significant. There were more additional POP room and hospital contacts for the percutaneous group. At 6 weeks plated patients had significantly better PEM and QuickDASH scores as well as range of motion, but not at later follow-up. Grip strength was better in plated patients at all times but this was not reflected in functional scores. There were no significant differences between the groups in Quality of Life scores at any point, and both groups had returned to baseline at 1-year follow-up. Interestingly there was no significant difference in time off work; the plate group took a median 37 days (10-132) and the percutaneous group 47 days (11-84, p=0.877) before returning to work.
When the overall costs of the two treatment options were compared, use of volar locking plates was significantly more expensive, with an additional mean cost of £713 per patient (SE 109.3, p<0.001).
The authors concluded that volar locking plates resulted in earlier recovery of function than percutaneous fixation but that there was no mid- or long-term functional benefit and no evidence of increased cost effectiveness.
My main concern is that all distal radius fractures are lumped together in this study; there is no analysis of specific fracture groups that may do better with plating, e.g. aged patients or intra-articular fractures. Another problem is that 21% of plated patients performed heavy manual labour compared to only 12% of percutaneously fixed patients and this may have distorted return-to-work figures for plated patients.
1. Percutaneous fixation with Kirschner wires versus volar locking plate fixation for adult patients with dorsally displaced fracture of the distal radius; randomised controlled trial
Costa ML et al. BMJ 2014;349:4807
2. Cost effectiveness of treatment with percutaneous wires versus volar locking plates for adult patients with a dorsally displaced fracture of the distal radius
Tubeuf S et al. Bone Joint J 2015;97-B:9:1082-89
Both of these papers come from the same Distal Radius Acute Fracture Fixation Trial (DRAFFT), a multi-centre randomised controlled trial of percutaneous Kirschner wire fixation compared to volar locking plates for 461 adults with distal radius fractures within 3 cm of the wrist. Intra-articular fractures that did not need open reduction were included; no patients had supplementary external fixation. Clinical outcomes were measured by the Patient Related Wrist Evaluation (PRWE), DASH and the EQ-5D-3L questionnaire at baseline, 3, 6 and 12 months after surgery. Information collected included use of health resources (admissions, OPD visits, plaster changes, medication, aids etc.) and use of personal social services (meals on wheels etc.). Time off work or loss of income were also included in the financial analysis.
Using PRWE, there was no significant difference in the rate of improvement after surgery between the two groups; scores were still about 15% below pre-injury levels at 12 months. There was also no clinically relevant difference between the techniques in patients above the age of 50 or intra-articular fractures. DASH scores were minimally statistically (p=0.051) better at 12 months after plating, but this was not clinically relevant. K-wire fixation required a significantly shorter theatre time (mean 31 minutes) but this was not included in the cost analysis. Patients treated with K wires needed more plaster casts and outpatient visits, but used less antibiotics. There was no difference in refracture, revision or debridement rates, and only minor insignificant differences in infections, nerve or tendon injuries and hardware removal between the two groups.

There was a mean additional cost of £714 per patient treated with a volar locking plate for an insignificant (p=0.013) increase in Quality Adjusted Life Years (QUALYs).

